What Is Considered a Reviewable Sentinel Event Specifically to a Behavioral Health Facility
Incident Reports
and Root Cause Analyses
2002-2008:
What They Reveal Well-nigh Suicides
View Adobe Acrobat Version | Download Adobe Acrobat Reader
June 2009
New York Country
Office of Mental Wellness

Michael F. Hogan, PhD
Commissioner
Lloyd I. Sederer, MD
Master Medical Officer
Jayne Van Bramer
Director, Role of Quality Direction
Amongst the reviewable sentinel events defined by The Joint Commission (TJC) is the suicide of whatsoever individual receiving care, treatment and services in a setting staffed around-the-clock or within 72 hours of discharge from such a setting. Incident reports submitted to the Office of Mental Health (OMH) reveal that this particular type of sentry consequence occurred 122 times between 2002 and 2008. To present this number in context, NYS inpatient mental health handling facilities operate approximately 3,660,000 bed days each year. Thus, limiting sentinel consequence (SE) suicides to approximately 17 a twelvemonth is indicative of the skilled work of the clinicians serving these individuals. This report uses OMH incident reports to nowadays historical data and a discussion of factors hospitals identified in their root cause analyses that may take contributed to the suicides or areas that otherwise called for improved performance. Every 1 of the 122 suicides is a tragedy that requires united states of america to acknowledge its high human cost in anguish and pain and have measures to prevent a similar recurrence.
Every suicide is a tragedy that requires u.s. to acknowledge its high human toll in anguish and pain and take measures to prevent a similar recurrence.
It is our intention that this SE suicide report volition nowadays an occasion for hospitals to review their policies and practices to ensure they are taking all measures reasonably possible to forbid this grave tragedy.
The Broader Motion-picture show
The most current in-depth analyses of national suicide data cover the years 2004 and 2005. The National Heart for Health Statistics reports that in 2005, 32,637 people committed suicide in the U.s., i.due east., 11 suicides for every 100,000 persons and one suicide every 17 minutes. Suicide ends the life of more persons each year than does homicide or
AIDSand
HIV-related illness. It is the fourth leading crusade of decease in persons 18-65 years of historic period. In New York Country during 2005, one,189 individuals ended their lives by suicide. This rate of 6.2 suicides per 100,000 persons ranked New York 49th amid the 50 states. While the depression rank is heartening, looked at from another perspective, one of every 27 suicides in the nation occurred in New York Land.
Information from Incident Reports


A review of the sentinel result suicides (inpatient or within 72 hours of discharge) reported to the OMH during the seven-year menstruum 2002-2008 indicates that the yearly totals take fallen within the narrow range of 12-22. The most contempo two years of the written report period, 2007 and 2008, showed the smallest number of SE suicides. The location of the suicides-on inpatient units vs. post belch or on laissez passer/AWOL-has shifted. In recent years, mail discharge suicides have significantly outnumbered in-hospital suicides. For purposes of this review, individuals who completed suicide while they were on laissez passer from an inpatient psychiatric unit or if they had left the inpatient unit without permission are counted with individuals who completed suicide inside three days of discharge. This allows us to look at factors affecting in-infirmary suicides every bit distinct from those occurring in the community, beyond the supervision of infirmary staff.
Every bit illustrated at left, in that location has been a steadily failing trend in the number of in-hospital suicides between 2002 and 2008 which may be due, at least in part, to vigilance in identifying and correcting ecology suicide hazards, as reported by the impacted hospitals' Root Cause Analyses.
Suicides of persons recently discharged or on pass/AWOL have deemed for over half of the SE suicides each year, except for 2002. In the years 2005-2008, these suicides accept represented 81 percent of the total study suicides as compared with 56 percent in the earlier three years. The American Association of Suicidology cites the month following discharge as highest risk, with about post belch suicides occurring in the week following belch.
Intuitively ane might surmise that shorter lengths of infirmary stays in recent years and increased reporting of post-belch suicides have likely impacted the increase, merely incident reports and root cause analyses indicate that systemic issues and the need to maintain clinical practice standards as well factor in this increase as described later in the study.
A Closer Expect at the 7-Year Data
As would be expected, given the far greater number of persons served past licensed programs, in each of the years studied more SE suicides were reported by these programs, as presented below. This is true of both in-hospital and postal service discharge/on pass/AWOL suicides for the study period 2002-2007. In 2008, the unmarried in-hospital suicide occurred in a state-operated facility. Ane in-infirmary suicide occurred in an Article 31 hospital, in 2007.
Gender, Age and Race
The National Institute of Mental Wellness (NIMH) reports that "almost four times as many males every bit females die by suicide."1 In four of the seven years studied, the OMH data reflected nearly the aforementioned or greater gender disparity than reported by NIMH. OMH incident data for SE suicides indicated that over the written report catamenia, the number of completed suicides involving women trended downward, despite the spike in 2007. At its highest, forty percent of the SE suicides were completed past women in 2002 and 11 per centum, the everyman, in 2006. Of the persons who died from in-hospital suicides during the study period, 11 (30 percentage) were women.
In contrast to the asymmetric number of men dying from suicide, no age grouping was spared, as axiomatic in the broad age range among persons in the study group. Overall, these persons ranged in age from 15 to 93. Nearly half (48 pct) of the SE suicides were completed by persons aged 31-l. In 2002, 2003 and 2008 no persons 75 or older were reported as having died equally a result of a sentinel event suicide. In contrast, the study group included one woman 93 years old who died past suicide in 2004, four persons in 2005 ranging in age from 75 to 85, an 87 yr old human in 2006 and a 77 year-old man in 2007. At the opposite end of the age range, the youngest individuals in the report were a 15 year-former boy who hanged himself on an inpatient unit in 2007 and a 17-year-old young woman who also died in 2007 of self-induced asphyxiation while on pass from the infirmary. The twelvemonth 2002 was noteworthy considering eight (40 pct) of the individuals who died from SE suicides were under age 30. Four of these young persons died on inpatient units-3 by hanging and one by overdose. Two were on pass or AWOL; 1 dying by hanging and ane from overdose. The remaining two individuals jumped to their decease after belch.
Of the 122 persons whose suicides were reviewed every bit sentinel events, 64 pct were identified as Caucasian, x percent equally African-American and 11 percent as Hispanic. Asians constituted six percent of this group. In total, 27 per centum of those studied were identified as persons of color. Consequent with data presented before, in all of the indigenous groups, suicides by males heavily outnumbered suicides by females. Caucasian males constituted the single largest category-57 percent of the total, followed by Caucasian females at 17 percentage.
| Ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | Total | Percent |
|---|---|---|---|---|---|---|---|---|---|
| Caucasian | 14 | 12 | 9 | 16 | 10 | 8 | 9 | 78 | 64 |
| African American | ii | 3 | two | 2 | ii | one | 0 | 12 | 10 |
| Hispanic | ane | 3 | 2 | 3 | 3 | ane | one | 14 | 11 |
| Asian | 2 | ane | 0 | 0 | 1 | 2 | 1 | vii | 6 |
| NA* | 1 | 1 | 2 | 1 | 3 | two | 1 | xi | 9 |
| Total | 20 | 20 | xv | 22 | 19 | 14 | 12 | 122 | 100 |
*NA=race data not available.
Suicide Method
Hanging and jumping from a height or in front of an oncoming vehicle were the most mutual methods of SE suicides in the vii years studied, equally the table beneath indicates. The number of persons jumping to their death has increased as the number of contempo discharge suicides has increased. Individuals who had been discharged within 72 hours or who were on pass or AWOL virtually normally completed suicide by jumping from a height or in front of a subway or heavy motor vehicle. This method accounted for 40 percent of these 85 deaths. Death from gunshot wounds (13 per centum) and drug overdose (15 percent)-in some instances street drugs, and in other instances prescription medications-were the next most mutual methods of suicide for this set of individuals.
| Method | Number | Percentage |
|---|---|---|
| Hanging | 37 | thirty |
| Jumping | 36 | 30 |
| OD | 17 | 14 |
| Gun | xi | nine |
| Cutting/Stabbing | 6 | five |
| Asphyxiation | 4 | iii |
| Drowning | i | 1 |
| Burns | 1 | one |
| Non Identified | 9 | 7 |
| Full | 122 | 100 |
| Location* | Number | Percentage |
|---|---|---|
| Bathroom | 20 | 54 |
| Bedroom | 11 | 30 |
| Shower Room | two | 5 |
| Solarium | 1 | 3 |
| Hall | i | 3 |
| Part building | 1 | iii |
| Not Identified | 1 | iii |
| Total | 37 | 101 |
*in-hospital or under staff supervision suicides
Of the 37 suicides completed on psychiatric inpatient units or outside the hospital just under the direct supervision of hospital staff (one event), 28 (76 percent) were completed by hanging. From 2005 through 2008 all of the in-hospital suicides were by hanging. Almost individuals who died past suicide on inpatient units concluded their life by hanging themselves using their bedroom door or a door inside their bedroom-a closet door or more unremarkably a bathroom door. Grab bars in the bathroom, a closet door handle in the shower room, and the frame of a stretcher each figured in one in-hospital hanging suicide. Since the means are available and questions related to individual privacy often confound decisions regarding level of supervision and monitoring, these are not unexpected findings.
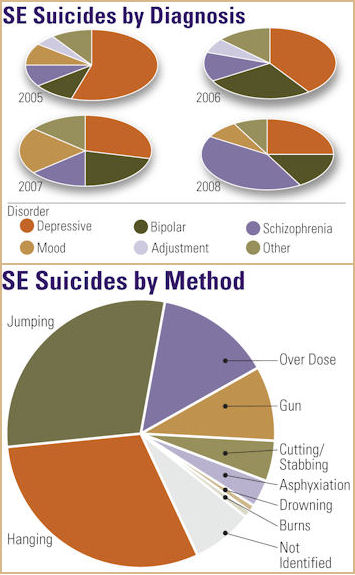
Methods of suicide over fourth dimension are represented at right.
Diagnoses Diagnoses were bachelor for 61 of the 67 persons who concluded their life by SE event suicides in the years 2005 through 2008. (Information on diagnoses was non bachelor for the earlier years of the written report). In reporting diagnoses, the beginning-listed principal diagnosis was selected. The findings indicate that 67 percent of these individuals were diagnosed with a mood disorder. These figures align with those of the American Foundation for Suicide Prevention and the NIMH both of which gauge that 60 percent of persons who take their own life have a mood disorder. Persons with a diagnosis of schizophrenia (several types) made upward 18 percent of the sample. Chronic hurting syndrome, anxiety disorder, alcohol and polysubstance dependence and body dysmorphic disorder comprised the "other" category.
Suicide Root Cause Analyses:
Findings and Lessons
Root cause analyses of the SE suicides identified areas in demand of improvement that included clearer and more than frequent communication, including record documentation, by physicians and clinicians; staffing allotment and training; environmental modifications; and changes in policies and procedures. As if taken from a Joint Commission report that in 2005 identified deficiencies in communication and patient assessments as ii of the most common contributors to inpatient suicides, root crusade analyses of the sampled suicides most oftentimes identified the demand to communicate effectively with families, other team members, and other treatment providers (and document that advice so that the information was available to all team members) and the importance of adopting or revising a suicide run a risk cess tool.
Inpatient Suicides
With few exceptions, all of the root cause analyses completed later in-hospital suicides identified opportunities for comeback in the suicide/risk cess process. These included the need to conduct and/or document a take chances assessment, the use of more than comprehensive suicide/risk assessment forms, and fully completed risk assessment procedure. Specific recommendations related to suicide run a risk assessments included:
- evolution of suicide risk assessment forms and grooming for psychiatrists and nursing staff in their employ. The purpose was not to provide a checklist to be completed, merely to prompt clinicians in their interviews to address all of the bug listed;
- enhancement of suicide risk assessments currently in utilise to discourage rote answers and ensure individualization. The risk assessment should address both dynamic and static adventure factors. Static risk factors might include age, gender, history of impulsivity and previous suicide attempts. Dynamic risk factors might include a review of the crisis that precipitated the admission, the presence of current suicidal ideation and the availability of means and emerging stressors.2 For example, the decision by the individual's mother, with whom he had been living, to not allow him to return was not listed as a stressor in the assessment in question. In some other instance, an individual working is this state on a work visa had recently lost his task. The handling team needed to take these circumstances into account and the individual's stress at believing he may be deported.
- policy change to require that suicide risk assessments be completed on access, once again at 72 hours, and within 48 hours of belch. The American Association of Suicidology (AAS) recommends that a risk-benefit analysis should be completed prior to decisions granting leaves, passes, and discharges for persons at high risk for suicide.
- modification to the suicide risk assessment to include a conclusion of risk level (low, moderate, high); and,
- expectation that suicide risk assessments volition be completed daily for inpatients considered at loftier risk.
These recommendations reflect the current standard of intendance that would take a suicide hazard assessment completed and repeated when clinically indicated, since the caste and intensity of suicidality is not constant. Clinical indications would include an precipitous modify in clinical presentation and the lack of improvement or gradual worsening of condition despite treatment.3
Several hospitals identified the need for physicians to write orders when supervision levels of individuals were recommended for change. In some instances, the team had agreed to the increase in supervision, but no order was written and with inadequate communication, the enhanced supervision did not occur on all shifts. Some other hospital revised its policies to require that all bachelor team members assemble to reach a decision on supervision status. Yet some other hospital implemented an updated running log of persons on enhanced observation status kept in a prominent place in the nurses' station as a useful tool for staff to quickly identify individuals who need staff members assigned to observe them.
The absence of a comprehensive access note that addressed past suicide attempts was noted every bit a cistron in several inpatient suicides. Some clinicians spoke of their reluctance to speak virtually suicide in an interview, lest the topic agitate the individual or for fright of introducing the suggestion. Dr. Shawn Shea, a former director of a psychiatric emergency department, states in The Delicate Fine art of Eliciting Suicidal Ideation that in his experience errors in suicide assessments often did not seem to stem from poor clinical decisions, but rather from expert clinical decisions based on bad data. The data most normally absent or distorted "related to the extent of the patient's suicidal history, planning, and current intent."4
Some hospitals identified a breakdown in the process of securing prior records or in communicating with the referring program. Hospitals acknowledged that treatment teams had not reviewed earlier hospital records, even when they were readily available at their own hospital. In response, staff training and memos followed, clearly articulating the expectation that prior records exist requested, secured and reviewed.
Several hospitals wrote procedures requiring the responsible staff member to contact mental wellness providers with whom an individual had had contempo contact. This recommendation was repeated oft, as hospitals, during the root cause analyses learned that staff had been operating with an inaccurate or incomplete moving picture of individuals' recent mental wellness status. This became particularly apparent when hospital staff learned also late that individuals had made previous suicide attempts. Several hospitals took other actions every bit well that included:
- instituting a checklist covering accessing historical records from all sources;
- developing a psychiatric transfer grade to be used to document verbal communication between the sending and receiving psychiatrists;
- requiring the completion of a psychiatric history timeline for all individuals with four or more than admissions. This timeline was to include information nigh diagnoses, medications, reasons for access, and belch arrangements; and,
- instituting structured interviews of family members to learn the family unit's and the individual's mental health history.
Many of the in-hospital suicide root crusade analyses identified environmental problems that were either a factor in the suicide or were identified every bit potential suicide hazards. Corrective actions included:
- changing door hinges to piano hinges;
- removing all plastic bags from units;
- replacing drop ceilings then that the plumbing/ventilation above is not accessible;
- enclosing the plumbing nether bathroom sinks;
- installing hallway mirrors;
- shortening television cables and nursing phone call button cables;
- locking tub rooms when non in employ;
- removing hanger bars from wardrobes and closets;
- installing no-gap grab bars in showers, push button on/off shower valves, and shower heads that will not back up a ligature;
- providing sturdier appliance for securing air-conditioners;
- attaching emergency number stickers to all phones in patient care areas;
- mounting door-endmost devices (V-shaped hinges a the top of the door) on the public rather than private side of the door;
- discontinuing the use of pajamas with ties or draw strings; and,
- using a weekly or semi-weekly Environmental Chance Cess Tool.
Other improvements taken in response to in-hospital suicides, not surprisingly, included efforts to increment the effectiveness of monitoring rounds and other supervision measures. Many of these measures were accompanied past policy and staffing changes. Cosmetic actions included:
- increasing monitoring of the dorm surface area. Several hospitals identified varying the monitoring schedule so that rounds are staggered and less anticipated.
- requiring that bedroom doors be kept ajar when individuals are resting;
- clarifying rounds procedures to include the requirements that staff observe an individual'southward motion during sleep, i.e., rise and fall of the chest, and take visual or verbal contact with the individual during daytime rounds;
- placing all newly admitted persons on every 15 minute monitoring
- for the beginning 24 hours;
- redesign of the medico coverage schedule and on-call procedures for weekends to increment coverage;
- assignment of specific staff members to monitor specific individuals who are on xv-minute checks;
- requiring staff to make verbal contact with and a response from individuals in the shower area during rounds;
- permitting the use of dark lights or red-filter flashlights to facilitate night checks;
- reduction in the unit of measurement census;
- implementation of semi-annual CPR drills to refresh staff'south skills. In this instance staff panicked when they found the individual unresponsive and did not immediately initiate CPR.
- initiating a special paging lawmaking for life-threatening emergencies to differentiate these from general calls for assistance;
- revising visitor search procedures to prevent the introduction of contraband items, specifically, in this instance, drugs; and,
- revising 15 minute monitoring forms to require that the staff fellow member document what the private was doing, non merely that he/she was nowadays.
In a particularly thoughtful root cause assay, the hospital identified the demand for training for staff to improve the quality of entries in the clinical tape to reverberate the uniqueness of the individual. Information technology called for work on eliminating records that just document the response to medications, daily routine, etc. and instead reflect time spent with the private getting to know and sympathise him/her. Similarly, another hospital identified the need to claiming the "people-pleasing, everything is alright mask" worn by some individuals with suicidal intent.
Mail Belch Suicides
Lack of Effective Communication
Similar to concerns identified in reviewing in-hospital suicides, the importance of communicating effectively with or enlisting the assistance of family members was cited every bit an area requiring improvement in many of the post discharge suicides studied. Inadequate communication with the family unit or no communication at all resulted in a lack of information or erroneous information nearly the family's and individual'southward mental health history. This issue, together with the need to improve the content and utilise of a suicide cess tool, were well-nigh often implicated in the suicides studied or were identified as areas that required improvement.
Several root cause analyses noted that the individual had denied the intent to harm him/herself and did not have a plan for self-harm. All the same, the clinician was not enlightened of the private's passive suicide ideas and repeated iterations, such equally, "I promise I don't wake up." Use of Case (Chronological Cess of Suicide Events) interviewing techniques might have elicited this data. In this interview, the clinician would explore in order suicidal ideation/attempts fabricated within the past 48 hours, then within the preceding two months, past suicidal ideation/attempts, and any suicidal ideation occurring during the interview itself.5
In several instances, hospital staff did non brand face-to-face contact with the family member with whom the individual would be residing at discharge. This resulted in insufficient exchange of data on such vital bug as:
- removal of guns from the home;
- the risks in mixing alcohol and psychotropic medication;
- the risks in taking prescription pain medication and psychotropic medication;
- increased suicide risk for persons who have attempted suicide in the by;
- the availability of contact crisis intervention services and how to contact the service; and,
- outpatient appointment information.
Grave consequences followed.
These deficiency findings led some hospitals to require that families sign a safety program for the private who was returning home with them. Other hospitals prohibited the apply of telephone interviews with family members unless a face-to-face meeting was impossible. At some other infirmary corrective measures were put in place to ensure that all team members had gear up admission to relevant information when it was found that the social worker had held an in-person meeting with an individual's family and had written a comprehensive note that included information relevant to the belch plan. That notation, nevertheless, was put in a bin for filing and did non appear in the tape until later the individual had been discharged and had died past suicide. Social workers now file their notes every bit soon as they are completed. Improving constructive communication skills was also the goal of recommendations for role-play preparation to increment the proficiency of receptionists, switchboard operators, security and other non-clinical staff in gathering data from families.
The need for improve communication with other providers of service, including the referring program, was identified at a frequency second only to the need to communicate effectively with families. By suicide attempts, family member suicides, and persistent suicidal ideation went unreported considering of these omissions. As noted earlier, some clinicians did not review handling records from their very ain facility. Tragedy ensued when a clinician did not speak with a private doc who was treating an individual and prescribing medication for chronic pain and in some other case when a substance abuse treatment provider were not contacted. One infirmary identified the need to coordinate its ain medical, detox and psychiatric services, and cited this as an expanse for improvement.
Risk /Suicide Assessments
While not negating the responsibility to perform a thorough psychiatric assessment, the need to introduce or revise a formalized, structured lethality assessment was identified in many of the root cause analyses completed following a suicide within three days of discharge. One hospital identified as factors to be considered- history of suicide attempts, risk factors, stressors, access to weapons/means, collateral information, and consultations with other providers. Often, the recommendation to develop or revise a run a risk assessment included the need for a policy that specified the circumstances and frequency with which the assessments must be completed. Specifically, several hospitals identified the need for a documented cess immediately prior to discharge or when at that place is any decrease in supervision status.
One infirmary in the study now requires that the Director of Inpatient Psychiatry review all individuals admitted on 1:1 supervision and determine when to reduce the observation level. Another hospital changed policy to direct that only physicians may behave lethality assessments. Hospitals' activity plans typically provided for staff training in the use of the assessment tool and monitoring the quality of the tools for a specific menses of time.
Falling nether the heading of self-axiomatic recommendations, 1 hospital made procedural changes that require a total team review of all high-risk individuals considered for discharge with a stay of less than vii days. Another hospital instituted a policy requiring a minimum 48-hour stay for individuals with "suicidal ideation, a programme and ways." Yet another hospital questioned whether the brusk length of stay of the decedent had provided sufficient time to accurately gauge the effectiveness of handling.
Handling Issues
Several of the suicides studied identified opportunities for improvements in treatment which resulted in changes in handling policies and practices. These addressed:
- securing and reviewing serum levels during rapid medication titration;
- medication trials of sufficient length to ensure clinicians could reliably judge the effectiveness of an anti-depressant medication earlier irresolute to another;
- establishing a standard of care for persons diagnosed with low;
- instituting a benzodiazapine detoxification protocol;
- guidelines for doing urine drug screens;
- expectations around the documentation of the upshot of PRN medications in the clinical record;
- tighter supervision of resident physicians' prescribing practices particularly during the first month of rotation;
- expectations effectually the timeliness and content of discharge notes by social workers and psychiatrists;
- clinical preparation for staff in therapeutic interventions using role playing and other active pedagogy techniques;
- changes in the CPEP discharge form to include documentation of health teaching and follow-up appointments; and,
- back-up review of physician discharge medication orders to ensure they are consummate.
The inability to form a bond with persons of a different culture and lack of appreciation of the mores of a particular culture were cited in the suicides of two persons of Asian and Middle Eastern descent. In one example, the facility acknowledged that arranging for interpreter services during therapy sessions was non sufficient to break the isolation of the private and allow staff to grade a bail with him. In some other example, clinical staff did not appreciate the touch of a young person'southward reconnection with his Center Eastern heritage and the change this engendered in the fashion he viewed those closest to him.
The inadvisability of Friday discharges and the lack of acceptable housing options figured in several causal analyses. 1 root crusade assay characterized shelter housing equally disheartening to individuals and as having an undermining result on all other components of the belch plan. The need to remain in the hospital considering the search for appropriate housing was taking too long led one man to leave the hospital confronting medical communication, and he died by suicide soon afterwards.
Decision
When this written report serves every bit a catalyst for word of interventions to reduce suicide risk and resolution to accept all steps possible to identify and support persons at take chances of suicide, it will have met its objective. The findings from this review support unequivocally the conclusion that comprehensive, thoughtful clinical hazard assessments founded on current, accurate and complete information from the individual, family members, past clinical records, and other treatment providers, repeated when clinically indicated and prior to key decisions, remains the strongest single tool in reducing the tragedy of SE suicides.
- AAS Guidelines Help Identify Chance of Suicide for Inpatient and Residential Patients
- J. Knoll, MD: Correctional Suicide Risk Assessment and Prevention. Correctional Mental Health Report, January/February 09.
- S. Shea, MD: The Delicate Art of Eliciting Suicidal Ideation. Psychiatric Annals, May 2004.
- S. Shea, Doctor: The Fragile Art of Eliciting Suicidal Ideation. Psychiatric Register, May 2004.
- Suicide in the U.S.: Statistics and Prevention, revised.
congdonancentiond.blogspot.com
Source: http://omh.ny.gov/omhweb/statistics/suicide_incident_rpt/
0 Response to "What Is Considered a Reviewable Sentinel Event Specifically to a Behavioral Health Facility"
Post a Comment